Mpox (monkeypox)
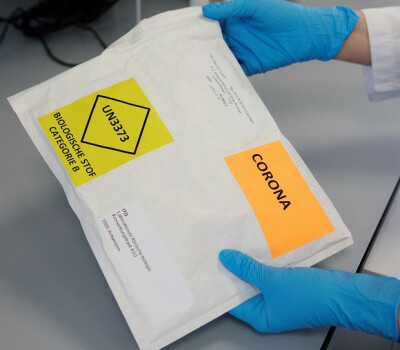
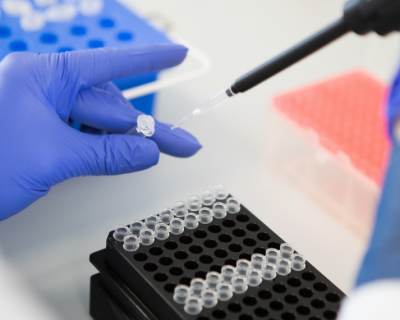
At the forefront of mpox outbreaks
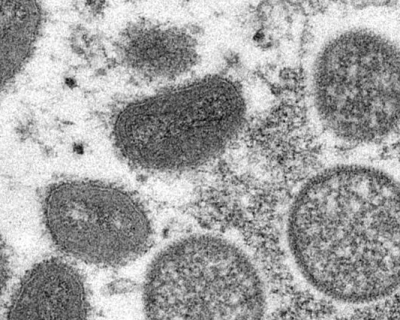
Mpox (genus orthopoxvirus), previously called monkeypox, is a variant of the virus that caused the "normal" smallpox. It was first discovered in 1958 in laboratory monkeys, hence the previous name. However, it is not certain that monkeys are the main reservoir (carrier) of the virus. According to the latest findings, these are more likely to be African rodents.
Until recently, the mpox disease was found mainly in forested areas in Central and West Africa, namely in the Democratic Republic of the Congo and Nigeria. Since May 2022, there has been a major outbreak outside the African continent. Particularly countries in Europe and North America have been affected, including Belgium.
Units
Labs
National Reference Laboratory (NRC) for Infectious and Tropical Diseases
FAQ
Were you at risk or do you have questions?