
Events
Discover upcoming events of ITM.
Loading
Upcoming events
Aula Janssens, Campus Rochus
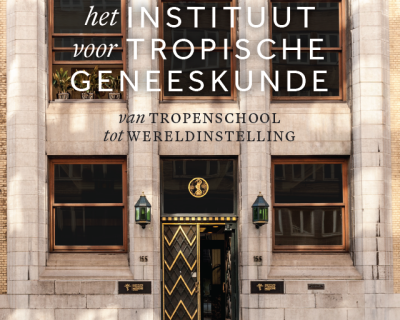
Book Launch: Institute of Tropical Medicine - From Specialist School to World-Class Institution
Past events

-
Campus Rochus, Sint-Rochusstraat 43, 2000 Antwerp
International Chemsex Conference: Optimising Support and Care for People Engaging in Chemsex

Live at ITM (Campus Rochus, Aula Janssens) and online
Decolonising Global Health & Education: A conversation with Dr Seye Abimbola

VU Amsterdam, Main Building, Aula, De Boelelaan 1105, 1081 HV Amsterdam, the Netherlands
PhD defence Christelle Boyi Hounsou

ITG Onderwijscampus Rochus, Aula P.G. Janssens, Sint-Rochusstraat 43, 2000 Antwerpen
PhD defence Elizabeth Tabitha Abbew
Ghent University, Faculty of Veterinary Medicine, Clinic Auditorium D, Salisburylaan 133, Merelbeke
PhD defence Salvator Minani

ITG Onderwijscampus Rochus, Aula P.G. Janssens, Sint-Rochusstraat 43, 2000 Antwerpen




