In countries like Niger, there is a painkiller shortage, not an addiction

Recent conflicts in Sudan and Niger have had devastating effects on people's daily lives and futures, including in terms of care and essential medicines. For instance, during the first weeks after the coup in Sudan, The Guardian reported on the "tragedy within the tragedy" of diabetes patients struggling to get hold of life-saving insulin and keep it at the right temperature while fleeing from homes that had suddenly become unsafe.
In the media, however, there is much less, or rather no, coverage of Sudanese and Nigerian patients with acute or chronic pain, and the associated question of whether the health system is still able to provide morphine and other essential painkillers in a timely manner (in addition to trying to address the needs of the many victims of the violence). But perhaps the following questions are more pertinent: were health systems able to provide pain medication at all before the conflict? And what will be the impact of the conflict?
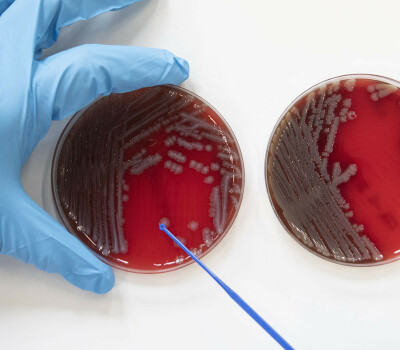
The answer is sobering. Medications such as morphine, also known as opioids, are essential for treating severe and/or excruciating pain. But if misused, they are addictive and prone to abuse. North America, for instance, has been hit by a were 'epidemic' of deaths caused by overdoses of fentanyl and oxycodone for several years.
This 'abuse crisis', mainly affecting high-income countries, is well known and extensively covered in mainstream and specialised media. However, there is also an 'access crisis', mainly affecting low- (or middle-) income countries, such as Niger and Sudan. The latter is often ignored by the media.
Clear gap
The recent report Left behind in pain, published in June 2023 by the World Health Organisation (WHO), illustrates the shocking inequality in access to morphine for medical use worldwide: in 2021, more than 80 per cent of it was used in North America and Europe - high-income countries are thus 'in pole position' when it comes to access to morphine.
Globally, there is a clear gap between consumption levels and medical needs. The WHO report acknowledges that access in poor countries is hampered by a number of factors, including legislative, infrastructural, etc. But central to the crisis is still the dual legal nature of opioids: policymakers fail to strike a balance between access for medical needs on the one hand and prevention of abuse on the other.
The somewhat thin line between medical use and abuse also seems to discourage many activists and journalists from talking about the unmet needs of adults and children in pain in low-income countries in the Global South.
The unequal access to morphine for medical use worldwide is ethically unacceptable.
Moreover, many efforts to strengthen health systems in the Global South prioritise disease prevention and treatment, inadvertently losing sight of people's wider needs, including pain therapy and palliative care. While there are attempts here and there to address the gap, these tend to be local initiatives, or those that are still at a preliminary stage.
For instance, the Ministries of Health of the Democratic Republic of Congo and Belgium, in collaboration with UNODC (United Nations Office on Drugs and Crime), have recently taken concrete action in this area, including on health worker training and awareness campaigns to address the issue. But it remains a huge challenge to scale up these local actions nationally as well.
Incidentally, it may be clear that the need for opioids increases abruptly during natural or man-made disasters, as in the current conflicts in Sudan, Niger, eastern Congo and elsewhere. But whether countries and regions are on fire or not, the unequal access to morphine for medical use worldwide, and the resulting human suffering, is ethically unacceptable and requires concerted action by policymakers, academics and politicians, with health and human rights at the centre of policy.
Raffaella Ravinetto is professor of pharmaceutical public health at ITM. Anselme Mubeneshayi Kananga is a consultant for the UN agency UNODC. And Xavier de Béthune is the former coordinator of Be-cause Health and medical director of Doctors of the World.
Spread the word! Share this story on