Even legally allowed amounts of antibiotics in food can cause resistance.
The presence of legally permitted antibiotic residues in food can lead to antibiotic resistance in humans. This is shown in a new study from the Institute of Tropical Medicine (ITM), published in Scientific Reports. For the first time, researchers have demonstrated that even very low doses of antibiotics that are legally approved and previously assumed to be safe can trigger resistance in bacteria in the human gut.
The research started from the observation that resistant bacteria appeared in people who had not used antibiotics for years.
Previous studies were mainly conducted in laboratories (in vitro), which does not always reflect what happens in the human body. This study is the first to test the effects of antibiotic residues in humans (in vivo).
According to the World Health Organization (WHO), antibiotic resistance is one of the greatest threats to global health. A new WHO report released on October 13 revealed that one in six laboratory-confirmed bacterial infections worldwide in 2023 was resistant to antibiotic treatment.
Antibiotics are used worldwide in livestock and fish farming. As a result, small amounts of antibiotics may remain in food, usually within the legally permitted maximum residue limits (MRLs). These limits are based on the acceptable daily intake (ADI): the amount of antibiotics that can be ingested daily over a lifetime without experiencing adverse health effects.
However, according to the study, even these permitted amounts can still be dangerous. Not because they are toxic to humans, but because they encourage antibiotic resistance in bacteria.
Clinical study confirms risk
In a randomized clinical trial, 20 healthy volunteers received the ADI of the antibiotic ciprofloxacin, which is widely used worldwide, daily for four weeks. A control group of 10 participants received a placebo.
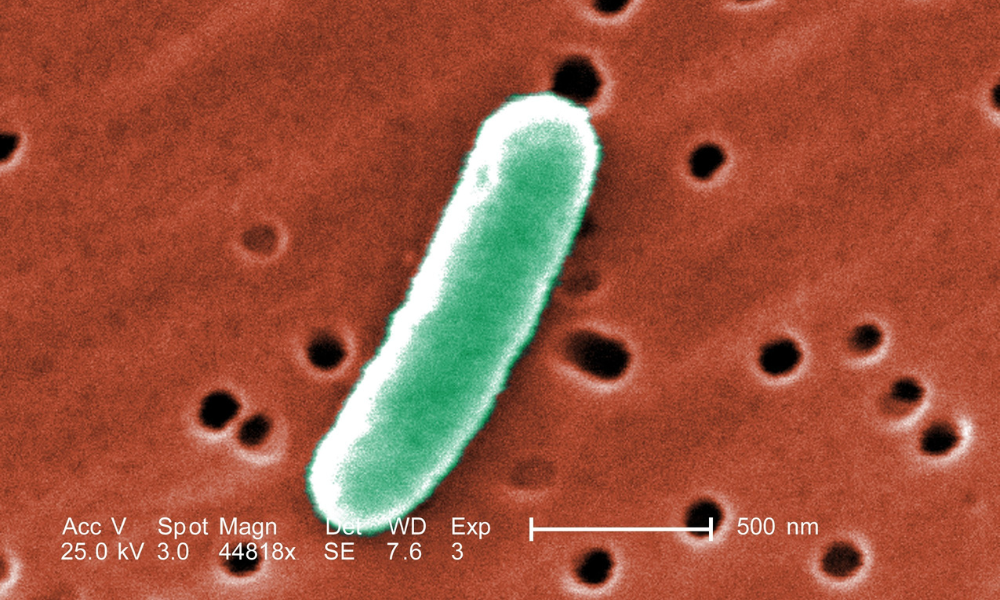
The results were clear: the amount of antibiotics that is currently legally permitted in food did lead to resistant bacteria in the participants. The researchers observed resistance emerging in Escherichia coli (E. coli), a widespread gut bacterium. In addition, the gut microbiome was disrupted: some beneficial bacterial species decreased, while others increased.
“Previous research has shown that the use of antibiotics in food animals can lead to resistant bacteria, which may then be transferred to humans. Our research points to a more direct cause: even small traces of antibiotics in our food can make the ordinary bacteria in our bodies resistant,” says ITM professor and last author of the study Chris Kenyon. “In other words: the problem does not only arise outside us, but also within us.”
Call for revision of standards
The researchers warn that current food safety regulations do not sufficiently take this risk into account. They therefore call for a revision of policy in order to slow down the rise of resistant bacteria.
Spread the word! Share this story on









