Mpox incidence nearly quadruples in 14 years

The number of mpox cases has almost quadrupled in the past 14 years in the Democratic Republic of the Congo. Children under five are particularly at risk. Rural populations are also particularly affected. An analysis by ITM and the National Institute of Biomedical Research (INRB) in the DRC, published in The Lancet, shows that the virus continues to spread and the way in which it is spreading continues to evolve.
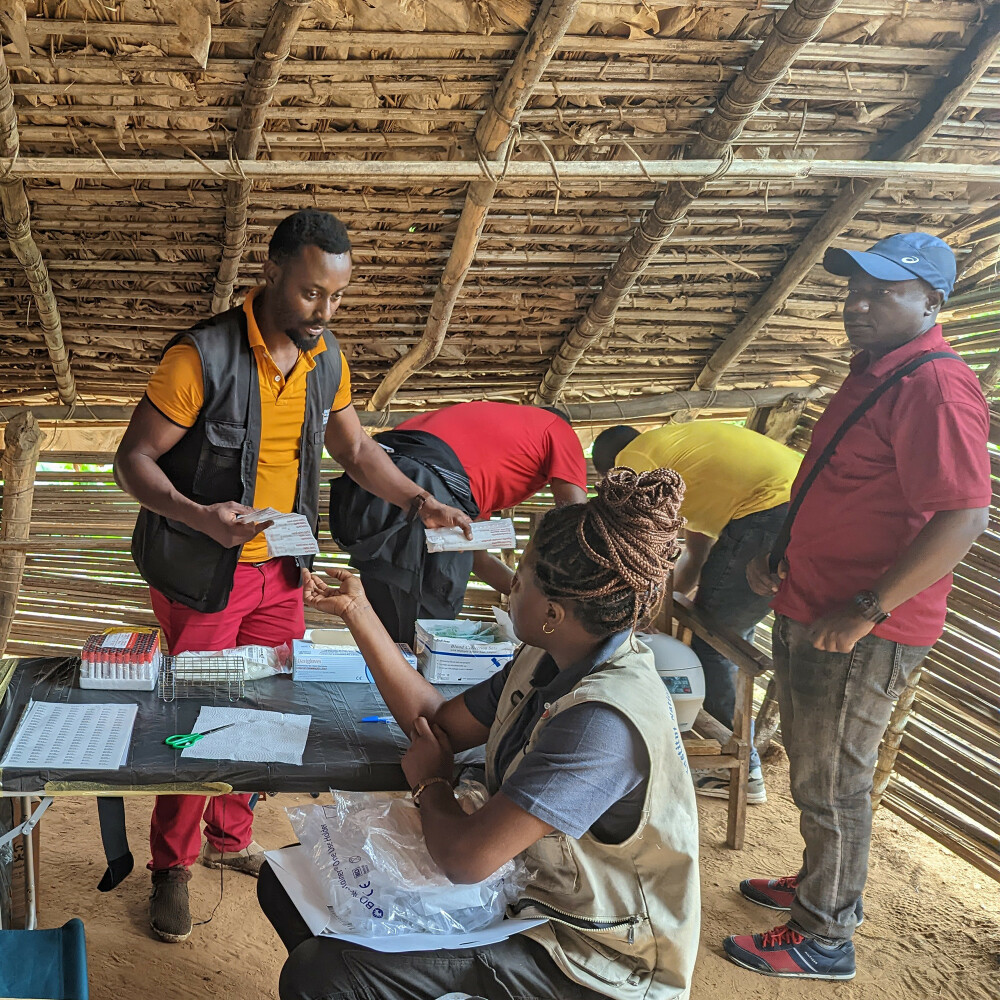
Header image, from left to right: Eugene Bangwen (ITM), Yves Mujula Kanundey (INRB), Elise De Vos (ITM), Bob Herady, and Christophe Van Dijk (ITM)
The study looked at nationwide surveillance and laboratory data between 2010 and 2023. During this period 60,967 suspected mpox cases and 1,798 suspected deaths were reported in DRC. Rural areas were significantly more affected than urban regions, with young children under the age of five experiencing the highest incidence and fatality rates.
One major driver behind the rise in mpox cases is the discontinuation of smallpox vaccination in the 1980s. The smallpox vaccine offered cross-protection against mpox, and its cessation has left populations increasingly vulnerable. By 2010, the steady increase in cases began to accelerate.
The analysis also noted a sharp decline in reported cases in 2021, likely due to disruptions in disease surveillance caused by the COVID-19 pandemic. However, cases rebounded significantly in 2022 and 2023. This systematic increase in cases over the years would ultimately culminate in the emergence of the new Clade Ib variant in 2024, which quickly spread across the DRC and to neighboring countries. As a result, WHO declared mpox an public health emergency of international concern.

Why we’re missing the full picture
Accurately assessing the full extent of the mpox outbreak remains challenging. Many cases go unreported because people in remote areas often do not seek medical care. Additionally, healthcare workers may struggle to identify mpox due to limited training. Poor infrastructure, including inadequate transportation and communication systems, further hamper data collection.
What’s driving the spread?
Although the exact causes of the disease are not yet fully known, several factors contribute to the spread of mpox. First, as forests are cleared and ecosystems disrupted, humans are coming into closer contact with animals that carry the virus. In 2023, more than 6,000 cases were reported in the heavily forested province of Equateur, where a major outbreak is currently ongoing. Second, while animal-to-human transmission remains significant, researchers are observing a rise in human-to-human infections, including through sexual contact. Finally, armed conflicts and displacement are facilitating the spread of the virus to new areas.
Global wake-up call
These findings underscore the urgent need for enhanced disease surveillance, targeted vaccination strategies, and robust public health interventions. Strengthening healthcare systems, improving the training of health workers, and addressing environmental factors such as biodiversity loss are critical to curbing the spread of mpox.
Full article
Read articleSpread the word! Share this story on