One year of mpox: from the African forest to the city


A looming threat
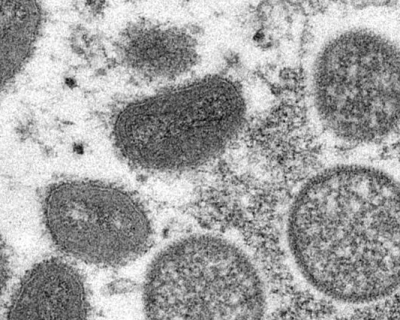
In the spring of 2022, an outbreak of mpox (formerly known as monkeypox) took the world by surprise. The virus caused more than 85,000 infections worldwide, predominantly affecting men who have sex with men (MSM). We know of two variants of the monkeypox virus. Clade I has previously caused multiple outbreaks in Central Africa, notably in the Democratic Republic of the Congo (DRC). This clade is often associated with severe skin rashes and has a fatality rate of 10%. Clade II, on the other hand, produces milder symptoms and has primarily been observed in West Africa. However, it was this second variant that spread extensively outside Central and West Africa, ultimately triggering a global outbreak.

Controlling the outbreak
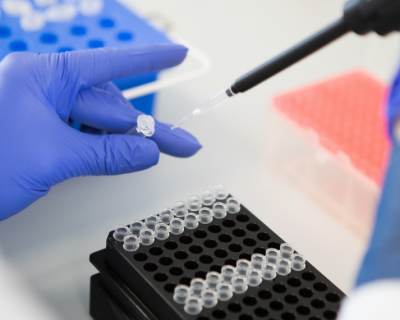
On 19 May 2022, we identified the first Belgian patient. With ultimately more than 790 confirmed cases, Belgium faced a severe outbreak. ITM played a crucial role in managing the situation thanks to our expertise in tropical viruses and extensive HIV and STI clinic. We informed individuals who were potentially exposed to the virus or displayed suspicious symptoms. We provided guidance and urged them to get tested. Moreover, we offered appropriate counselling and advice to those who tested positive. "Since our colleagues were already working on mpox in the DRC, we were able to rapidly implement a diagnostic PCR test in the Clinical Reference Laboratory," explains molecular biologist Dr Jasmine Coppens.
In an effort to contain the spread of the virus and speed up the new vaccination campaign, our doctors shared their expertise in the intradermal vaccination technique with other HIV centres. This technique enabled them to optimise their vaccine supply and help more people at risk. "Considering we administered these microdoses at two different times, we were able to preventively vaccinate 2.5 more people at risk. As a result, we made a huge leap forward compared to the first phase of the outbreak," says Dr Patrick Soentjens, head of the ITM travel clinic. “As of 22 November, Belgium had sufficient vaccine stocks, which enabled us to return to vaccinating via the original technique.”

Understanding the epidemic
The clinic played a crucial role in effectively managing the outbreak, but alongside that, our researchers undertook significant efforts to gain a deeper understanding of the epidemic. The collaboration between the clinic and the research team proved invaluable as they shared their expertise and supported each other throughout the process. Doctors and nurses actively participated in research meetings, while researchers provided valuable guidance and insights to the clinicians. "By analysing the virus DNA, we discovered that we were dealing with variant II of the virus," says Dr Koen Vercauteren, clinical virologist. "Shortly after the initial diagnosis, we even found evidence of asymptomatic infections in individuals who visited ITM's HIV and STI clinic for gonorrhoea and chlamydia testing," adds Dr Marjan Van Esbroeck, head of the Clinical Reference Laboratory.
These findings, which were published in Nature Medicine, gathered international interest.
In a parallel study, physician-researcher Dr Isabel Brosius and her colleagues looked at infection risk following high-risk contacts. Participants in the study provided daily samples and kept a detailed diary, documenting any physical symptoms they experienced. This approach allowed us to identify new infections early and see who became infected and when they developed symptoms. The study revealed two significant findings. Firstly, it demonstrated that the risk of virus transmission is significantly higher after sexual contact, compared to other forms of close contact. This highlights the importance of addressing the specific risks associated with sexual exposure. Secondly, the study showed that asymptomatic patients can also shed the virus before they have symptoms and therefore before they know they are ill.
The findings from this study had a substantial impact on global public health recommendations. Leading institutions such as the World Health Organisation (WHO) and the Center for Disease Control and Prevention (CDC) and the European CDC updated their guidelines based on our research. For instance, they now recommend that individuals who have had a potential sexual exposure to the virus should refrain from engaging in sexual contact for a period of three weeks following the exposure.
"Interestingly, a patient tested positive a few days before the first detected symptomatic case in Belgium. This person had not been travelling or attending a mass meeting, indicating that the virus was already circulating in Belgium before the first diagnosed case,"
Dr Irith De Baetselier
Lead researcher of the study
Support ITM research
Our mission is to deliver science for worldwide health, an endeavour to which you can contribute as well. By giving to ITM, you help us face the most pressing global health challenges of today.

Fighting the stigma
Mpox quickly replaced coronavirus in the media as a new infectious threat, and social media was flooded with a stream of hate messages against gay people. Our doctors and researchers condemned the stigmatisation of the gay community in De Morgen newspaper. In this case, they were among the first victims, but it is impossible to predict where the next virus will strike. HIV research teaches us that involving the affected community ensures respectful and effective communication of new insights. The community is not the problem, but rather part of the solution.
Currently, the mpox study group is looking at the hypothesis that the sudden drop in infections was triggered by network immunity. This means that the outbreak died out because infected men with many alternating sexual partners became immune or temporarily did not have sex, thus eliminating connecting links in the sexual network that caused the outbreak to die out.
"We are currently working on serological and modelling studies to determine whether this hypothesis is correct," says Dr Christophe Van Dijck. "In the meantime, we should be aware that future outbreaks of mpox may occur if network immunity is disrupted. This can happen, for example, by declining immunity of infected or vaccinated individuals or when previously uninfected, peripheral members of the sexual network become more sexually active."

Meanwhile in the DRC
In collaboration with the Institut National de Recherche Biomédicale (INRB), our partner in the DRC, we have investigated several outbreaks in the country. In the DRC, the monkeypox virus predominantly circulates amongst animals in the rainforest. However, the virus has made cross-species jumps with alarming regularity, leading to outbreaks amongst humans. We are currently working with INRB on a large multidisciplinary research project on the dynamics of mpox transmission, clade I.

Outbreak preparedness at ITM
This outbreak is not the first of its kind, and unfortunately will not be the last. Globalisation, global warming, biodiversity loss and urbanisation have increased our vulnerability to infectious diseases. To adequately address these challenges, it is imperative that we prepare ourselves and continue to invest in infectious disease research. By doing so, we can better equip ourselves to tackle future outbreaks and safeguard public health on a global scale.
Research themes

Mpox
Read moreSpread the word! Share this story on