
Evenementen
Ontdek aankomende evenementen van het ITG.
Laden
Aankomende events

-
Campus Rochus, Sint-Rochusstraat 43, 2000 Antwerp
Internationale Chemsex-conferentie: betere ondersteuning en zorg voor mensen die aan chemsex doen
Aula Janssens, Campus Rochus
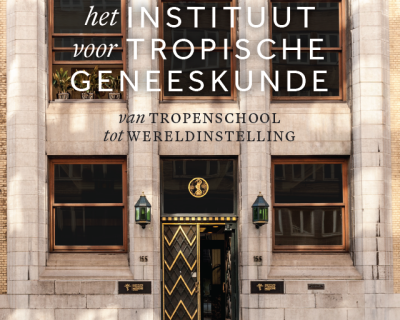
Boekvoorstelling: Instituut voor Tropische Geneeskunde - Van tropenschool tot wereldinstelling
Afgelopen events

Live at ITM (Campus Rochus, Aula Janssens) and online
Dekolonisatie van Onderwijs en de Wereldgezondheid

VU Amsterdam, Main Building, Aula, De Boelelaan 1105, 1081 HV Amsterdam, the Netherlands
PhD defence Christelle Boyi Hounsou

ITG Onderwijscampus Rochus, Aula P.G. Janssens, Sint-Rochusstraat 43, 2000 Antwerpen
PhD defence Elizabeth Tabitha Abbew
Ghent University, Faculty of Veterinary Medicine, Clinic Auditorium D, Salisburylaan 133, Merelbeke
PhD defence Salvator Minani

ITG Onderwijscampus Rochus, Aula P.G. Janssens, Sint-Rochusstraat 43, 2000 Antwerpen




